Vacuum Bell Therapy is a non-surgical treatment option for pectus excavatum, a pectus deformity that causes the chest to appear sunken or caved in. If you have pectus excavatum and want to avoid surgery, then vacuum bell treatment could be a good option.
The Vacuum Bell works by using a silicone cup and a vacuum pump (normally a hand-pump) to create an area of low pressure over the sunken part of the chest. The pump sucks the air out of the device which in turn creates a vacuum that pulls the depressed sternum and ribs outward. Over time, this pressure gently reshapes the chest and guides the sternum back to its normal position.
A daily exercise programme is prescribed alongside vacuum bell therapy for pectus excavatum to enhance the effectiveness of the treatment. Your orthotist will develop an individualised exercise programme to support the vacuum bell therapy. In addition, you can join the weekly sessions online with Alva Yoga which our patients enjoy, not least because it clearly indicates that they are not confronting their condition alone.
Vacuum bell therapy is a great option for people with pectus excavatum as it’s non-invasive and does not carry the risks of surgery.
The key for success of vacuum bell therapy is the flexibility of the chest. Naturally therefore, it is most effective at correcting the condition in pre-adolescent and adolescent patients, as they are still growing, and the chest wall is at its most flexible at this stage. However, it is quite possible to treat adults successfully as long as they have a flexible chest. LOC has devised a way of assessing an individual’s chest wall flexibility which can be done remotely during the free virtual pectus consultation.
A key part of our pectus excavatum treatment is the use of the rib flaring brace in conjunction with the vacuum bell. This treatment has been pioneered by LOC, addressing the whole chest shape by also correcting rib flaring, very often an associated deformity. The rib flaring brace enhances the power of the vacuum bell by acting as a lever point. LOC will carefully design the brace to work alongside the vacuum bell and ensure the positioning is optimum throughout treatment.
The vacuum bell was invented by Eckart Klobe, a graduate in Chemical Engineering. He used an early prototype of his invention to fix his own funnel chest before having the final version of his invention patented in 2002. It has been used successfully in the non-surgical treatment of pectus excavatum by many German, Austrian and Swiss clinics over the last decade and is slowly being recognised in the UK.
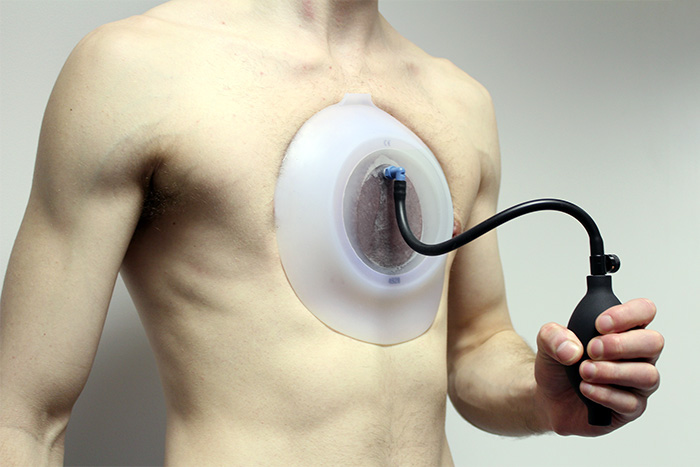
Patient demonstrating the vacuum bell and hand pump in action
For any treatment that requires a patient to follow a specific wearing regime, compliance to that regime will have a direct impact on the success of the treatment. The amount of change achieved will be affected by age, chest flexibility and how sunken the chest is to start with.
LOC’s advice is to wear the cup for two to three hours immediately after the completion of the daily exercise programme. This is when the chest should be at its most flexible and will maximise the effect of the correctional forces of the vacuum bell. We are also carefully managing patients through longer wearing times to help achieve better results. LOC’s treatment for Pectus Excavatum takes about a year to 18 months.
It's recommended to discuss all treatment options with your orthotist to determine the best course of action for each individual case of pectus excavatum.
This depends on several factors; the position of the chest wall deformity, its severity, the flexibility of the chest, the kind of results wanting to be achieved and the age of the person undergoing treatment for pectus excavatum or pectus carinatum.
Early adolescence (roughly between the ages of 12-16 years old) – is an optimum age to start treatment, given that the chest is still maturing, and flexible, permanent correction is more easily achievable. Once bracing treatment is complete and a patient has stopped growing, the deformity will not return. For younger pectus patients, conservative bracing is used to keep a deformity from worsening and can help them to avoid surgery in later life.
For older pectus patients (between the ages of 20 to 30) results can be harder to achieve, as the costal cartilage hardens into the bone as a person matures. Over the years we have successfully treated many adults for both pectus excavatum and pectus carinatum and active adults with flexible chests can expect good results.
If you are worried about your chest shape, or your child’s chest shape, then get in touch for a free Skype consultation with one of our pectus specialists who can assess their chest and discuss treatment options. We are always happy to communicate with local GPs, thoracic surgeons and consultants if a patient approaches us for bracing treatment after considering other options.
Again, this hugely depends on what a patient wants to achieve from treatment; whether that’s avoidance of surgery, improvement in the appearance of the chest shape, reduction in rib flaring etc. All these goals are taken into consideration during your first consultation. While there are no serious health risks of having pectus carinatum or excavatum – beyond the cosmetic – for many patients and parents, treatment outcomes involve improving confidence and self-esteem. During our 2018 Pectus Patient Survey, 92% of pectus carinatum patients surveyed said that treatment had a ‘major improvement’ or ‘an improvement’ on their social life.
You can read the results of our 2018 Pectus Patient Survey and quality of life questionnaire here.
Regular reviews are part of the treatment programme, preferably in clinic with one of our specialist orthotists, or via Skype consultations.
The number of appointments needed will vary from patient to patient but as a general rule, younger pectus patients who are growing at a faster rate will need to be seen more regularly for check-up appointments. This is to ensure that the brace fits well and is guiding the chest into the correct position as growth spurts occur. For other patients, this can be scaled back according to their individual needs and demands.
Regular appointments are beneficial for assessing progress, checking for signs of rubbing and determining whether another brace is needed. Appointments are also good for checking patient compliance to brace wearing and the breathing and exercise programme. At each appointment, we make time for patients to see our physiotherapist to fine-tune their exercise programme and check to see how a patient has been managing with the current programme.
We always advise coming in for appointments whenever you have any concerns about the brace or treatment programme, especially if a brace is rubbing or not fitting correctly. At the London Orthotic Consultancy, we have treated numerous international patients that have benefitted from specially designed braces that leave room to accommodate for growth and that can be adjusted remotely. Follow-up appointments for international patients are conducted via Skype.
It is really important to continue exercising while going through bracing treatment. Exercise is fundamental to keeping the chest wall flexible. Our treatment programme incorporates a daily exercise routine of around 30-40 minutes of stretching using yoga poses, resistance bands, deep breathing exercises and general muscle stretches. Deep breathing exercises allow the lungs to expand against the chest wall, pushing it outwards.
Exercising with the brace on in the later stages of treatment can also make the chest correction more stable and permanent.
Swimming is one of the best forms of exercise to complement bracing treatment, as the body positions required to swim imitate the resistance band training designed to stretch the chest and increase its flexibility. Some swimming strokes are better for this than others, please check with your clinician. The brace should always be removed for contact sports and for swimming.

“It’s life-changing, my swimming coach has even remarked what a difference my treatment has made" Read how pectus bracing treatment helped to correct Aris' complex chest deformity, involving a combination of pectus excavatum, pectus carinatum and rib flaring.

Cerebral palsy patient Lucas sees significant improvement in his walking after only six months in his new custom Ankle Foot Orthoses (AFOs), designed by Professor Saeed Forghany in our Manchester clinic. Hear how a detailed gait analysis and bespoke AFOs significantly improved Lucas's gait and comfort.

Freddie’s positional plagiocephaly was treated successfully with the LOCBand Lite, going from 11mm to 2mm after four months in his helmet.

Adult club foot (talipes) patient Natasha says, "I cannot stress how amazing my AFOs are and how they have changed so much for me. The support they give me allows me to walk without crutches outside the house for the first time in over fifteen years."

Diagnosed with adolescent idiopathic scoliosis at 14 years old, Polly and mum Zoe looked to the LOC Scoliosis Brace to help her curve and avoid surgery at a later date.

LOC opens its first clinic in Northern Ireland, LOC Belfast, offer non-surgical orthotic treatment for scoliosis, pectus carinatum and pectus excavatum. Here, we will also be able to provide orthotic treatments for a range of adult and paediatric lower limb conditions including cerebral palsy, spina bifida, hypermobility, stroke, post-polio syndrome, and multiple sclerosis.

Mum Natalie shares her experience of having both her identical twins diagnosed with craniosynostosis. Ella and Nina had surgery at Great Ormond Street Hospital before going through cranial remoulding therapy at the London Orthotic Consultancy.

See how a thorough gait analysis and a correctly-fitted, bespoke Reciprocating Gait Orthosis (RGO) helped Ted, a spinal surgery and cancer survivor, improve his rehabilitation and mobility goals, getting him back on his feet again.