
13 May 2019
When patients are undergoing treatment for scoliosis, they often ask our scoliosis specialists questions about which lifestyle changes they can make to help alleviate symptoms, make the most out of bracing or reduce the likelihood of their spinal curve progressing. Those with severe scoliosis curves may experience difficulty sleeping due to aches, pain and inflammation.
Below are some of the most common questions about chairs, furniture, sitting positions and mattresses, asked by patients undergoing treatment, with LOC’s Schroth-Certified physiotherapist to answer them.
There are many mattresses and pillows out there that use the terms ‘orthopaedic’ and ‘postural’ that purport medical benefits for back pain and scoliosis sufferers. Our advice would be, don’t be conned by the term ‘orthopaedic’ as, in relation to mattress products, this simply means ‘to support the joints, muscles or body’. The term ‘postural’ simply means ‘position of the body’.
This is a commonly asked question, though the answer really depends on what your issues are. Although a bad mattress won’t worsen your curve, it may aggravate symptoms of scoliosis, and the right mattress can help alleviate discomfort. Most of the time, a few simple modifications and adjustments can help as mattresses tend to lose their upper layers of support over time.
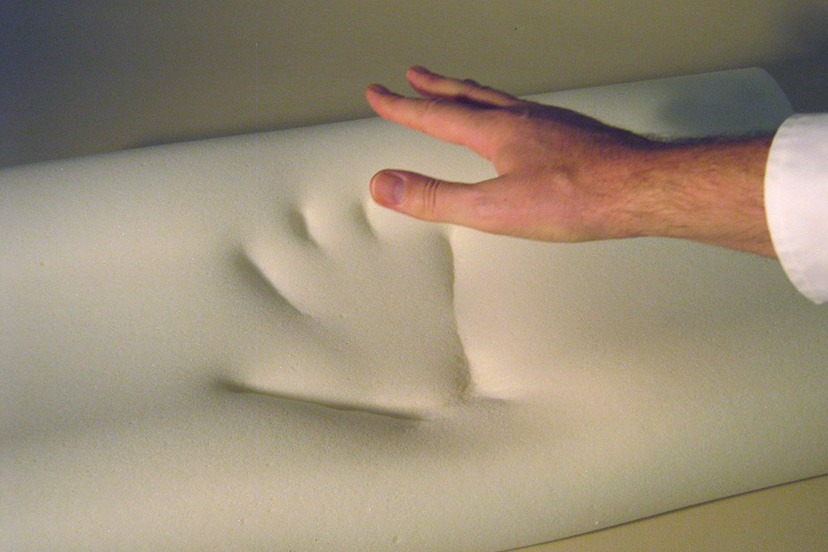
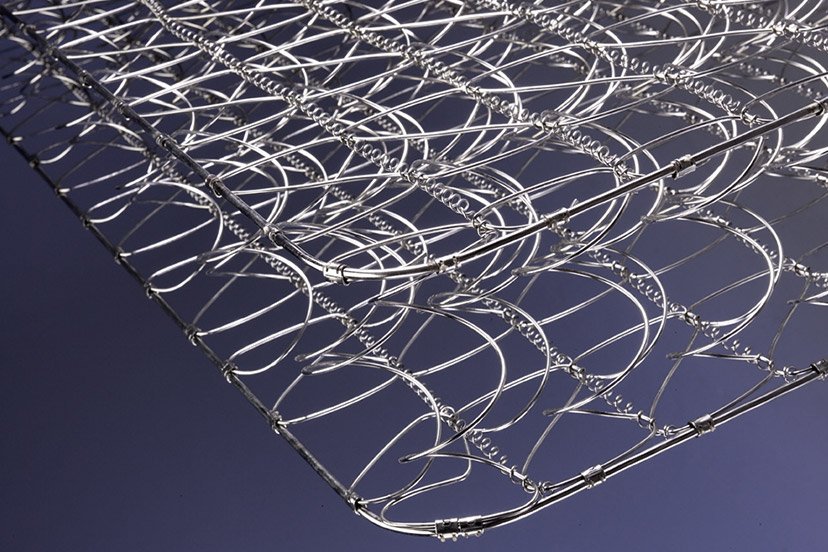
If you have scoliosis and do not suffer greatly from pain and are relatively mobile then the general advice I would recommend when buying a new mattress is buy as many pocket springs as affordable, go for medium to hard firmness for support and a layer of memory foam for comfort. If you upgrade the firmness of your mattress, you may need to upgrade your pillow at the same time or you could end up with a painful neck.
While a soft, cushiony mattress may seem appealing, a medium to firm mattress will keep your spine supported. Scoliosis is a curvature of the spine and conservative treatment (i.e. bracing and physiotherapy) broadly aims to return it to a straighter position. A firm, supportive mattress and pillow that supports your spine into a flat position is best. Memory foam is helpful for increasing comfort, as a medium to hard mattresses can feel unbearable to some, but an entire memory foam mattress will deprive your spine of support.
With adults, it’s often more important how we sit and the daily activities we do that keep the spine extensors and bones loaded and strong. If you suffer from chronic back pain (chronic meaning it’s lasted for over six weeks) then you may need to try out different types of mattresses to see what helps your symptoms and what you can tolerate. Most mattress companies offer a risk-free trial period of around 90 days, so this could be worth exploring. If you have mobility issues, again, your needs will likely require a more complex assessment with a specialist.
For scoliosis sufferers, a new mattress with as many pocket springs as affordable is a good place to start.
We don’t recommend a specific product to patients at present, just the guidance above.
Another common question - though you would need to be assessed by a physiotherapist to be sure advice is suited to you. Scoliosis treatment at the London Orthotic Consultancy is entirely bespoke; the Cheneau-Gensingen brace is tailored to each curve as well as the breathing and Schroth-based physiotherapy exercises. Sleep positioning will likewise be specific to the type and severity of scoliosis.
Another popular question. The simple answer, again, is it depends on what your issues are. There are many seating products that claim to reduce back pain although the majority are extremely costly as they’re made with expensive material and manufacturing costs.
My general advice, for those without mobility issues or complex medical needs is:
If you’re tall – small, short-legged chairs will automatically cause you to slouch. If possible, go for a chair with a seat that reaches your knee height level or higher.
If you’re short – you’re more likely to struggle to reach your feet to the floor and will therefore perch and slouch at the edge of a chair. The deeper the chair the more likely this will happen so try to find one with a shallow seat.
Take regular breaks and consider postural advice from a physiotherapist to help offload certain postural muscles.
Our specialist Scoliosis clinic in our headquarters clinic in Kingston, though we also offer a Schroth physiotherapy clinic at The Portland Hospital in central London. You can make an appointment at any of our scoliosis clinics by calling 020 8974 9989.
The operation used to treat severe scoliosis curves is typically spinal fusion surgery; a major procedure that involves moving muscles and realigning the skeleton into place. The curved, deformed vertebrae are fused together into a single bone, putting metal screws and rods into the spine to help straighten it. Surgery typically lasts between 4 and 8 hours depending on the severity of the curve. Bone graft is then taken from other parts of the body and used to cover the implants.
Following the operation, it is necessary to spend around a week in intensive care before returning home and the first few days are often uncomfortable. Most adolescents can expect to return to school from 2-4 weeks following surgery, but pain medication may be required up to 6 weeks following. A full recovery from the procedure can take up to a year, as it can take that long for the spine to heal fully.
Spinal fusion surgery causes the fused portion of the back to become permanently stiff, as a result, returning to sports that require large amounts of flexibility (ballet, yoga, gymnastics, dance) or contact (rugby, football, karate, hockey) may take longer.
Risks of spinal fusion surgery are like that of any other major procedure and include infection, blood clots and anaesthesia complications. The added risks include permanent nerve damage to the spine and paralysis.