Adolescent idiopathic scoliosis (AIS) represents over 80% of all diagnosed cases of scoliosis in children. Scoliosis can progress quickly when the skeleton is still growing or during hormonal changes.
Skeletal maturity occurs at the age of approximately 14 to 17 for females and 18 to 22 for males when the bones and spine are no longer malleable. If started young enough and depending upon maturity and magnitude of curvature, scoliosis bracing treatment can reduce the curve and Cobb angle and significantly reduce the requirement for surgery in later life.
Visible improvements in posture and rib hump after just 4 weeks of wearing the Cheneau-Gensingen brace. Mild cases of scoliosis may self-correct as a child grows. However, it is important that any existing curvature is monitored closely to check progression, particularly during periods of rapid growth during puberty.
For more serious cases (Cobb angles in excess of 25 degrees) we recommend non-surgical treatment with our bespoke version of the Cheneau brace, the LOC Scoliosis Brace.
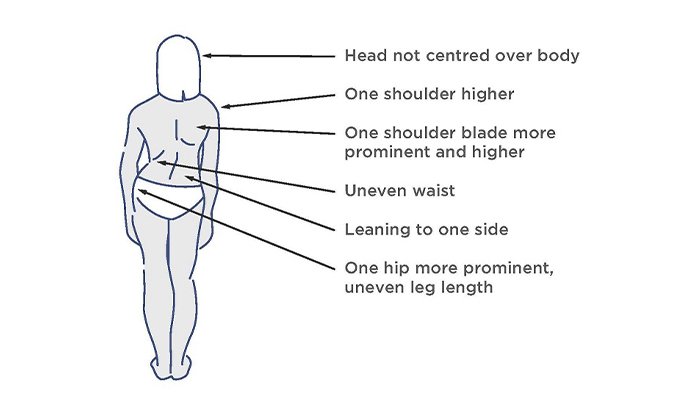
The visual signs of scoliosis
The patient pictured was diagnosed with adolescent idiopathic scoliosis at the age of 14 during a rapid growth phase. She had a thoracic curve of 35 degrees and was referred by a specialist for a spinal brace to manage her condition conservatively. After 6 weeks of wearing a bespoke Cheneau-Gensingen brace her curve in-brace had reduced to 12 degrees.

If your child has been diagnosed with scoliosis, you will naturally want to know whether the curve will get worse particularly if your child has not reached full maturity.
A number of scientific studies have established a risk factor or formula to estimate the risk of scoliosis progression for children with idiopathic scoliosis. In general, the more growing a child with scoliosis has to do; the greater the chance is that their scoliosis will get worse. As a young child’s skeleton is immature and can undergo rapid periods of growth during puberty, their scoliosis can rapidly progress during these growth spurts.
For instance, a 2017 study found that at the beginning of puberty, children with curves greater than 30 degrees had a 100% risk of progression to what is within surgical range (>45 degrees); while children with curves 21 – 30 degrees still had a 72.5% risk of progressing to that stage. (source: Charles, Yann Philippe; Daures, Jean-Pierre; Rosa, Vincenzo de; Diméglio, Alain (2006): Progression risk of idiopathic juvenile scoliosis during pubertal growth
Based on the magnitude of a curve present in a child at a particular stage of skeletal development, we can predict their likelihood of progression. Because every child is different, age does not directly correspond to a given stage of puberty, so one needs to factor in a combination of bone/skeletal age (determined by Risser sign), age, and the Cobb angle of the curve.
LOC can calculate the risk for you if you provide the following information:-
Please send the information to: [email protected], with the subject line: Scoliosis risk of progression calculation
One of our scoliosis clinicians will respond promptly and if it looks like your child does have a significant risk of curve progression, treatment options can be discussed in an initial free virtual assessment

See how a thorough gait analysis and a correctly-fitted, bespoke Reciprocating Gait Orthosis (RGO) helped Ted, a spinal surgery and cancer survivor, improve his rehabilitation and mobility goals, getting him back on his feet again.

We are proud to announce the launch of our latest innovation in non-surgical treatment for pectus deformities. Our new dynamic chest compressor is one of the slimmest pectus braces on the market and is designed to reshape the chest without the need for invasive surgery.

Rosie’s very severe plagiocephaly was no problem for the LOCBand Lite 3D-printed cranial remoulding helmet, going from 16mm to 2mm in just six months.

When John came to see us, his ankle was in a bad way. He had around 60mm of his tibia missing and not much if any talus present. He needed crutches to support him to walk. A gait analysis and a new bespoke carbon fibre knee ankle foot orthosis (KAFO) later and he is able to walk again without crutches.

Matilde travelled from Chile to LOC for bracing treatment for her adolescent idiopathic scoliosis. Now, nearly a year and a half since she started wearing her brace, she has achieved near-total correction of the curvature of her spine. This is her scoliosis bracing story.

After only 6 months of wearing bespoke pectus braces from The London Orthotic Consultancy, Will started to notice a visible difference in his pectus carinatum.

After trying out several scoliosis braces in Romania, Ukraine and Turkey, Iulia begins treatment with the LOC Scoliosis Brace and is already seeing results in a matter of months. Here her mum, Raluca, describes how and why they came to LOC for her treatment.

Through bracing treatment with the dynamic chest compressor, Jack has achieved 90% correction in his pectus carinatum after only two months. Here, mum describes Jack's non-surgical treatment journey.