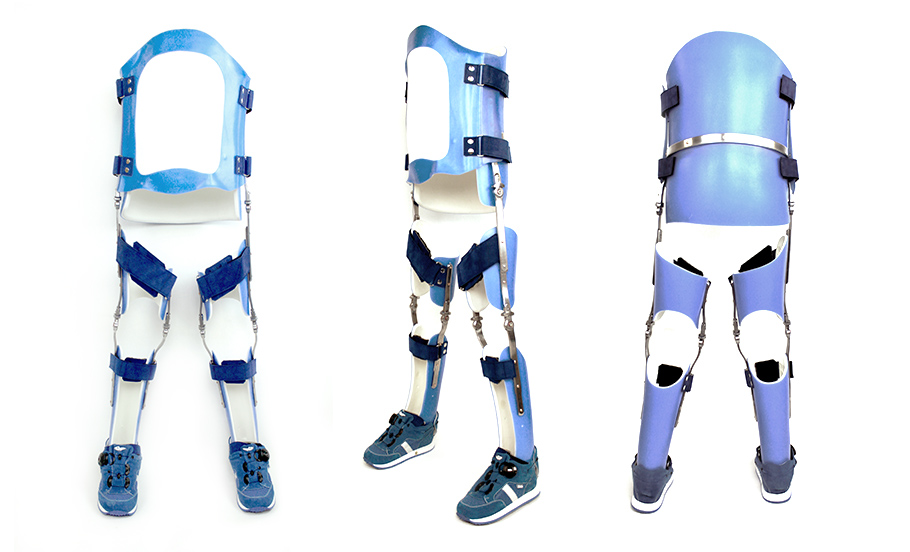
A Reciprocating Gait Orthosis (RGO) is a type of orthopaedic device used to aid individuals with mobility impairments, particularly those with lower limb weaknesses or paralysis. The primary purpose of an RGO is to help a patient to walk by providing support to achieve a reciprocal gait pattern.
The device typically consists of jointed metal frames, straps, and other components that attach to the user's legs and torso. The key feature of an RGO is its ability to mimic the natural walking motion. It allows for a reciprocating gait, meaning that as one leg moves forward, the other leg simultaneously moves backward, creating a more natural walking pattern.
RGOs include hinges at the hip and knee joints, allowing for a more dynamic and coordinated movement. They also incorporate a locking mechanism, providing stability during standing or resting phases.
The user usually initiates the movement by shifting their weight or using assistive devices. The RGO then translates this motion into a coordinated walking pattern, supporting the user's legs and facilitating a more independent and functional gait.

Reciprocating Gait Orthoses (RGOs) are commonly used for individuals with mobility impairments or paralysis in the lower limbs due to various medical conditions.
Some of the conditions for which RGOs may be prescribed include:
1. Spinal Cord Injury (SCI): RGOs are often recommended for individuals with spinal cord injuries, particularly those with incomplete injuries who have some residual mobility.
2. Cerebral Palsy: People with cerebral palsy, a group of neurological disorders affecting movement and coordination, may benefit from RGOs to assist with walking.
3. Spina Bifida: Individuals with spina bifida, a congenital condition where the spinal column does not close completely, may use RGOs to support ambulation.
4. Stroke (Hemiplegia): For individuals who have experienced a stroke and have weakness or paralysis on one side of the body (hemiplegia), RGOs can provide support for walking.
5. Guillain-Barré Syndrome: RGOs may be considered for individuals recovering from Guillain-Barré Syndrome, a condition that affects the peripheral nervous system.
6. Muscular Dystrophy: Some forms of muscular dystrophy, which are progressive muscle-wasting conditions, may lead to the use of RGOs to maintain mobility.
7. Traumatic Brain Injury (TBI): Depending on the extent and location of the injury, individuals with traumatic brain injuries may use RGOs to assist with walking.
It's important to note that the suitability of RGOs depends on the individual's specific condition, functional abilities, and rehabilitation goals.
A thorough assessment by healthcare professionals, such as orthotists and physiotherapists, is necessary to determine the most appropriate assistive device for each patient.
At LOC, we specialise in the use of RGOs. Our clinical team is experienced in the assessment and fitting of these complex orthoses. We manufacture the devices in our Kingston clinic, giving us excellent control and the ability to provide the best possible care.
RGOs typically require plaster of Paris casting. However, our clinical team has developed a 3D scanning process so that casting is not required thus reducing any stress and discomfort. We have also designed the orthosis within our Computer Aided Design (CAD) programme. This improves the alignment and fitting process and produces a better orthosis.
Once fitted, the RGO will require maintenance and optimisation throughout its life. LOC has on-site teams to service it, and we use our video vector gait laboratory to continuously optimise the alignment to ensure that our patient’s rehabilitation continues to progress.

Nine-year-old patient Ted with his bespoke Reciprocating Gait Orthosis and his walker with LOC Director Sam Walmsley, who made it for him.
We have the following facilities and amenities at our Kingston Upon Thames location:
We also have the Gait Laboratory for orthotics patients and Onsite Manufacturing for speedy turnarounds and adjustments whilst you wait.
An insole is a contoured orthotic device which alters the characteristics and biomechanics of the foot and ankle area. Biomechanics are concerned with mechanical laws and how they affect the living body, especially the musculoskeletal system.
They are removable devices, often made from plastic, that are designed to fit inside a shoe to provide additional support for your feet. As well as offering shock absorption, an insole can help distribute the weight of your body more effectively across the foot and can be made bespoke to cover a range of biomechanical conditions.
If you have symptoms in your feet, ankles, hips or your lower back that are intermittent or were not there to start with in early life, and have started to cause you pain over a period of time, bespoke orthotic insoles could be an excellent option.
If you have already tried rest, icing, compression and elevation and your feet have not recovered, we recommend a biomechanical assessment to consider the possibility of insoles. They are a non-invasive approach to treatment and in many cases, are a great option for symptoms that are not severe enough to warrant surgical intervention. Alternatively, they can be considered as an option prior to surgery.
We will send patients away when an insole is not appropriate, if a patient is suffering with iliotibial band syndrome for example, the problem can be helped with physiotherapy and a stretching programme. That’s what our biomechanical assessment is all about; determining whether there would be any benefit from altering the alignment of your feet.

Among 14 to 17-year-old cricket players, there is an increased risk of pars stress fracture, or spondylolysis, which can cause lower back pain and reduced mobility. These athletes are at high risk due to their still-developing bones, which struggle to cope with the repetitive stress of fast bowling.

Apprentice orthotist Catherine Hendy’s journey into the world of prosthetics and orthotics began in an unconventional way. After completing a degree in art, she then trained as an orthotics technician, before taking up an apprenticeship to become a clinician. Now, she’s been nominated for the British Association of Prosthetists and Orthotists (BAPO) Student of the Year 2024.

Amelia was diagnosed with tightness in her neck by her GP before her plagiocephaly diagnosis. Clinician Jo Drake treated her with a LOCband Lite cranial remoulding helmet, which improved her overall head shape and asymmetry.

What are lower limb orthotics, and how can they improve mobility and reduce pain? We've put together this summary of the different kinds of lower limb orthotics, from AFOs and KAFOs to more complex orthotics like RGOs, and how they can help patients with their mobility goals.

Barney's very severe flat head syndrome (plagiocephaly) and diagnosis of torticollis led to successful helmet therapy with the LOCband, significantly improving his head shape, going from 27mm asymmetry to 12mm.

“It’s life-changing, my swimming coach has even remarked what a difference my treatment has made" Read how pectus bracing treatment helped to correct Aris' complex chest deformity, involving a combination of pectus excavatum, pectus carinatum and rib flaring.

Cerebral palsy patient Lucas sees significant improvement in his walking after only six months in his new custom Ankle Foot Orthoses (AFOs), designed by Professor Saeed Forghany in our Manchester clinic. Hear how a detailed gait analysis and bespoke AFOs significantly improved Lucas's gait and comfort.

Freddie’s positional plagiocephaly was treated successfully with the LOCBand Lite, going from 11mm to 2mm after four months in his helmet.